Prostate MRI Prior to Biopsy Reduces Unnecessary Biopsies and Lowers Risk of Missing Significant Cancer
Recent Studies Support an MRI-First Protocol Which Can Provide More Accurate Information
According to the American Cancer Society, 1 in 8 men will be diagnosed with prostate cancer during his lifetime. Currently, prostate cancer is the second leading cause of cancer death in American men, second only to lung cancer. What’s more, since 2014, the incidence rate of prostate cancer has increased by 3% per year overall, and about 5% per year for advanced-stage prostate cancer.1
And yet, despite these statistics, success rates for prostate cancer treatment are actually higher than many other types of cancer. The 5-year survival rate in the United States for men diagnosed with prostate cancer is 99%. Today, more than 3.3 million men alive in the United States have been diagnosed with prostate cancer at some point.1
This data points to the fact that while the diagnosis and treatment procedures of prostate cancer continue to advance and evolve, the numbers of men actually participating in regular, potentially life-saving screening is still quite low.
What are the Screening Recommendations for Prostate Cancer?
The American Cancer Society advises men to discuss prostate cancer screening with their physician so that they can make informed decisions. The ACS advises having these discussions at:
Age 50 for men who are at average risk.
Age 45 for men at high risk. This includes African American men and men who have a first-degree relative (father or brother) diagnosed with prostate cancer younger than age 65.
Age 40 for men at even higher risk. These are men with more than one first-degree relative who had prostate cancer at an early age.
Following this discussion, men who want to be screened will receive the prostate-specific antigen test, familiarly known as the PSA test. This is a blood test that looks for prostate-specific antigen, a protein found in the prostate which when elevated, may indicate prostate cancer.
Historically, men with elevated PSA levels are referred for a biopsy to determine if the cause is cancer and/or if a tumor is present. However, accumulating studies are supporting an MRI-first prostate cancer screening protocol, in which MRI is performed after PSA screening and before biopsy. These studies are showing that having an MRI first provides more accurate information before proceeding to the biopsy.
A recent study published in Diagnostic Imaging2 found that implementing MRI prior to biopsy can actually help reduce unnecessary biopsies and lower the risk of missing clinically significant cases.
“The main benefits of MRI first is level-one data proves it can reduce by roughly 20% the men who don't need a biopsy, as their gland doesn't harbor any tumor,” explains Dr. Robert Princenthal, board-certified radiologist and Medical Director of RadNet’s Prostate MRI program. “We can identify more clinically significant prostate cancer, and help optimize individualized treatment pathways based upon more accurate staging of tumor volume and aggressiveness."
Researchers in the study noted that the use of MRI resulted in a high diagnostic performance for detecting clinically significant prostate cancer, with an 88% sensitivity rate and a 64% specificity rate. These numbers are crucial for guiding biopsy decisions, as Dr. Princenthal mentioned, as well as minimizing unnecessary procedures.
According to Dr. Princenthal, this study and others like it are part of the growing evidence to support what he explains as “prostate MRI plus PSA screening, in order to optimize early detection.”
“Radnet is recognizing how important screening for prostate cancer becomes in populations at increased risk, including many minority groups,” Dr. Princenthal says. “Cost has been an impediment, as well as lack of access to quality prostate MRI centers. Radnet is in planning stages to develop a low-cost screening 'mano-gram' without IV contrast, in association with a robust prostate AI detection tool. This will overcome cost-based objections to providing for men the benefits women have obtained for years with quality breast cancer screening with mammography.”
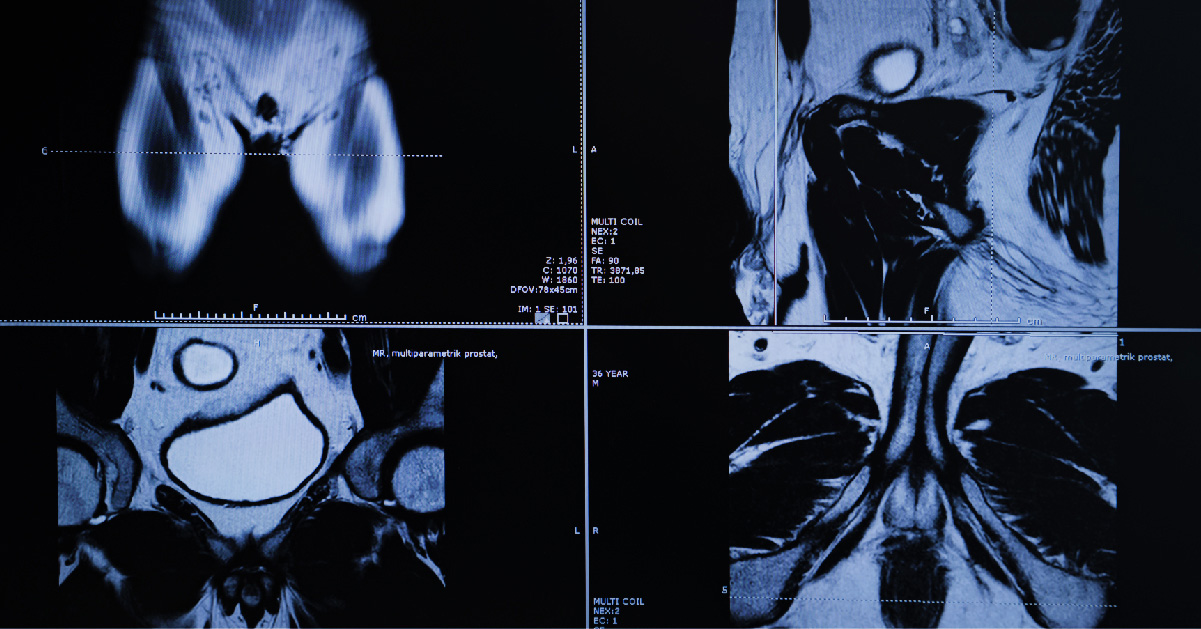
What is a Prostate MRI?
An MRI (magnetic resonance imaging) uses magnetic and radio waves to produce detailed images of soft tissues and structures in the body, such as the prostate. A prostate MRI exam takes about 25-30 minutes to complete.
Using magnetic waves to “take pictures” of the inside of your body, a prostate MRI is totally painless and non-invasive. Prostate MRI is accurate for detecting cancer as well as determining how advanced a cancer is and if it has spread to other parts of the body. A prostate MRI can also detect other prostate conditions such as benign prostate hyperplasia (BPH).
Dr. Princenthal encourages men to speak with their doctors about PSA and MRI screenings, saying that “the ability of evidence-based medicine to accurately screen, stage and treat prostate cancer has never been better.”

