What is Nuclear Medicine?
Nuclear Medicine uses very small amounts of radioactive materials (also called radiopharmaceuticals) to diagnose and treat disease. Radiopharmaceuticals are substances that are attracted to specific organs, bones or soft tissues.
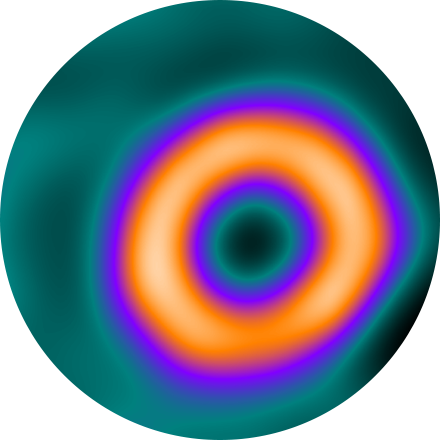
The radiopharmaceuticals used in Nuclear Medicine emit gamma rays that can be detected externally by special types of cameras. These cameras work in conjunction with computers to form images that provide data about the area of body being imaged.
While X-rays image the body’s anatomy, Nuclear Medicine shows actual organ function and physiology.
When is Nuclear Medicine used?
Nuclear Medicine uses radioactive materials to help diagnose a variety of diseases and disorders, and to assess how different parts of your body are functioning. Nuclear Medicine imaging can be used for many applications, including but not limited to thyroid disease, cardiac function, orthopedic injury and infection, blood clots in the lungs, liver and gall bladder function, and response to cancer treatment.
What happens during a Nuclear Medicine procedure?
During the procedure, you are given a low-level radioactive compound, called an isotope, which may be injected intravenously, inhaled or swallowed. The isotope accumulates in the organ being examined. Depending on the exam, your technologist may ask you to return later, sometimes many hours later or the following day, to give the isotope time to distribute to the area of concern in your body.
The organ to be examined will emit radiation continuously during the exam. This radiation is then detected by a special camera and subsequently processed through a computer. Patients typically do not experience side effects or allergic reactions since most of the compounds used in Nuclear Medicine are naturally-occurring substances in the body. The length of the exam varies, depending on type. You will be able to communicate with the technician during the procedure.
What are the benefits and risks?
Nuclear Medicine is non-invasive. It allows clinicians to get medical information that would not be available otherwise, or that would require surgical intervention. It is safe and painless, using very small doses of radioactive materials to diagnose and treat disease. The amount of radiation from a Nuclear Medicine procedure is often comparable to that received during a regular X-ray exam. Nuclear Medicine provides a valuable view of the structure and function of internal organs.
Some Nuclear Medicine Imaging Procedures Include:
The hepatobilliary system includes the liver, gallbladder, cystic bile duct and the common bile duct. A HIDA scan helps clinicians diagnose issues in those organs. The HIDA is used when an ultrasound exam is inconclusive, or when the patient is allergic to iodinated contrast. Generally, the logistics are the same as those described on this page, except if your doctor orders a CCK HIDA. This test reveals gallbladder function and requires a medication (injected) or special solution (which you drink).
A lung scan helps clinicians examine your lungs using a radionuclide and X-rays. A radionuclide is injected, and a camera can image how that liquid circulates in your bloodstream, specifically the supply to your lungs. You might also be asked to breathe a small amount of radionuclide mixed with oxygen through a face mask. The camera records where the air is going inside your lungs.
A nuclear “stress test” takes images of your heart at rest and after your heart has been “stressed.” The two are compared to reveal if there is any damage to your heart muscle. This procedure helps evaluate coronary artery disease, acute chest pain, hibernating myocardium and cardiomyopathies. Initially, you will be injected with an isotope, and (30 minutes later) resting images will be acquired. The stress portion is next, which involves either a treadmill or injection of medications that mimic physiological stress. A second isotope is injected for this portion of the test. After your heart rate returns to normal and you eat, the technologist takes the final set of images of your heart.
A renogram uses small amounts of radioisotopes to measure the function of the kidneys. This test evaluates the size, position, shape and function of the kidneys. A renal scan is particularly useful when there is a known sensitivity to the contrast media used in an IVP or other X-rays, or when there is underlying kidney insufficiency (reduced kidney function, as after a transplant). A renogram may be used to evaluate kidney function in people with hypertension or to check for rejection after a transplant.
A three phase bone scan is a nuclear medicine test, it uses radiotracers that are injected (or inhaled or swallowed). The radiotracers are detected by a special camera to provide pictures to diagnose a fracture when it cannot be seen on an X-Ray. It is also used to diagnose bone infection, bone pain, osteomyelitis, as well as other bone diseases.
This exam is most commonly used for diagnosing metastatic disease or primary bone cancers. It may also be used to diagnose Paget’s disease, fractures (old vs. new or post trauma), unexplained bone pain, and other bony abnormalitites.
The procedure itself is non-invasive and simple. The patient receives an intravenous injection of a radiotracer. There are virtually no side effects or allergic reactions to this or any other radiopharmaceutical. The patient may leave after injection and return approximately 3 hours later for the scan. You’ll be asked to lie still on a table while an armlike device supporting a tracer-sensitive camera passes back and forth over your body. Patients are encouraged to stay well hydrated to improve the images. Otherwise they may resume their normal routine. The whole body bone scan takes approximately 45 minutes to one hour for most patients.
Because the radiation dose comes from the injection not the camera, additional images may be obtained of any area of interest, sites of pain, etc. without additional exposure for the patient.

