Breast cancer is the second most common cancer in women (after lung cancer). Early detection of breast cancer vastly increases survival rates. Scheduling an annual mammogram after the age of 40 (or earlier, depending on your breast cancer risk factors) is one of the most important things women can do to ensure to take control of their health.
Some Breast Imaging Procedures Include:
Some women — because of their family history, a genetic tendency or certain other factors — should be screened with MRI in addition to mammograms. The number of women who fall into this category is small: less than 2 percent of all the women in the United States. Talk with your doctor about your history and whether you should have additional tests.
Breast MRI helps to detect small lesions sometimes missed by mammography — without using radiation or compressing the breasts. MRI uses powerful magnets and radio waves to take very clear pictures of soft tissues, so it can be extremely useful in breast imaging.
Ultrasound uses sound waves instead of X-rays to exam breast tissue. A transducer is passed over the breast. The transmitted sound waves are translated into a picture on a monitor. It does not cause discomfort and, because it does not use radiation, it carries very little risk.
Ultrasound is useful for women with dense breasts or for evaluating suspicious areas seen by mammography or felt during a breast exam. It can also find breast lesions that are close to the chest, where mammography is less useful. Breast ultrasound can distinguish between cysts, which are fluid-filled, versus other types of solid breast masses.
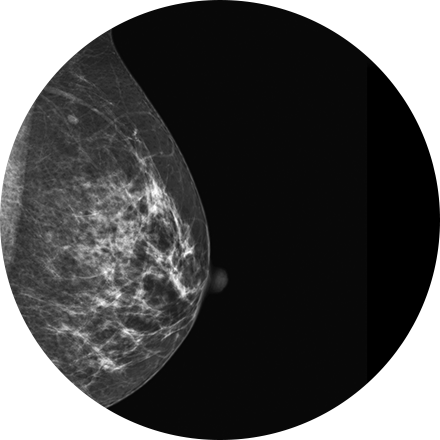
Mammography is a type of low-dose X-ray of the breast. It reveals masses and micro-calcifications within and around the breast that may indicate breast problems including, but not just limited to cancer.
Experts recommend a mammography screening of the breasts at regular intervals to increase the chance of early cancer detection and treatment. The American College of Radiology recommends women aged 40 and older should have a screening mammogram every year and should continue to do so for as long as they are in good health.
3D mammography (tomosynthesis) is an FDA-approved technology that complements conventional 2D mammography. While traditional mammography generates 2D images, 3D mammography creates multiple thin 3D image slices that allow each section of the breast tissue to be seen more clearly.
New imaging software used with our 3D mammogram units enables us to offer a lower-dose 3D exam. The software eliminates the need to obtain additional 2D images as part of the 3D exam, as previously required. This reduces the radiation dose, making it similar to that of a traditional 2D mammogram.
A 3D mammogram looks and feels like a regular mammogram. An x-ray arm scans over your breast taking multiple 3D images at various angles. Each scan takes about 4 seconds and the entire 3D mammogram lasts about 15-20 minutes.
MRI-guided biopsy uses MRI to guide the radiologist to the exact location of the area of concern. MRI biopsy is usually used when the abnormality can be best seen on breast MRI, but not as well visualized on mammogram or ultrasound. Often lesions that are biopsied are done under the imaging modality that best demonstrates them.
Image-guided biopsy allows patients to avoid hospitalization and general anesthesia (previously necessary with traditional surgical biopsy). It is a valuable method of getting a fast, accurate, conclusive diagnosis—without unnecessary time, pain or expense to the patient.
Stereotactic biopsy uses mammography to precisely guide clinicians to a lump or abnormality such as an area of calcification, that cannot be felt or seen on ultrasound. Clinicians see a 3D picture of the lump’s exact location.
Image-guided biopsy allows patients to avoid hospitalization and general anesthesia (previously necessary with traditional surgical biopsy). It is a valuable method of getting a fast, accurate, conclusive diagnosis—without unnecessary time, pain or expense to the patient.